In 2002 the results of a landmark and controversial clinical study known as The Women’s Health Initiative, or the WHI were reported. This study had enrolled older women (average age 63) who were many years past their menopause to assess the answers to very specific questions regarding the risks and benefits associated with hormone therapy (HT) for women after menopause.
The WHI was notable for its size with about 16,000 women participating and being divided into 2 study groups. Group 1 consisted of about 8000 women within an intact uterus.They were given a combined oral conjugated estrogen and a synthetic progestin known as Prempro. In group 2 the women had had an hysterectomy and were only given an oral conjugated estrogen known as Premarin without the progestin. There was a control group of women who were given a placebo without any hormone. Both Prempro and Premarin are not bio-identical hormones as the estrogen comes from horses and the progestin is completely synthetic. The term “bio-identical” refers to the same exact estrogen found in women such as estradiol or the progestin progesterone.
Prior to the WHI, physicians strongly believed that HT (bioidentical or not ) protected women from heart attacks, strokes and dementia over the long run. Concern over risks such as breast cancer and blood clots were down played mainly because earlier results of a large scale epidemiologic study of relatively young nurses. These healthy young women entering their perimenopause and menopause had started HT (not bioidentical) in their late 40s or early 50s for symptoms such as hot flashes, sleeplessness, poor memory and reduced quality of life. After initiating HT, yearly reports about their health and quality of life were collected. The results were impressive. The nurses seemed free of any chronic diseases such as diabetes, hypertension, high cholesterol or arthritis and they were quite active and vital. The nurses reported minimal side effects or serious illness.
The results of the WHI had a major impact on clinical practice as the study reported there was no heart attack, stroke or dementia protection in the women given HT in both groups 1 and 2. In group 1 there was a small increase in breast cancer compared to the control group. Interestingly in group 2, comprised of the hysterectomized women given estrogen only, there was actually a 33 percent decrease in breast cancer ( yes even with the non bioidentical estrogen ). Both groups seemed to have increased blood clots and both had some benefit in the form of bone protection against post menopausal osteoporosis and colon cancer.
Nevertheless, NIH stopped the group 1 study citing the lack of benefit in the presence of increased blood clots and breast cancer. However NIH also allowed the group 2 to continue as there had been a decrease in breast cancer. Unfortunately so many women in group 2 were alarmed at the scary and sensational reporting over the findings in group 1 pertaining to breast cancer that many women in group 2 dropped out of the study. With the members of study group 2 now down to an insignificant number, NIH closed it down the following year.
Following the results of the WHI, many doctors and medical specialty organizations advised against the use of HT for women at menopause believing HT to be more risky than helpful in most situations.
While the hormone treatments in the WHI were not bioidentical, the FDA applied the same warning label to bioidentical hormones considering all forms of estrogen and all progestin’s to be equally dangerous and on beneficial as those studied in the WHI. This is another controversial area related to the results of the WHI i.e. to the results of clinical studies using non-bioidentical hormones apply to bioidentical hormones?
The intense media reporting, much of it inaccurate, created great anxiety among women. This led to a 70% World-wide decline of menopausal HT with almost universal recommendations from physicians and medical specialty organizations for women to avoid HT if possible or use HT at the lowest dose and for the shortest amount of time. Following the 2002 WHI results, a generation of doctors, doctors in training, medical students and allied health personnel were “warned “ not to advise women there were any long term health benefits associated with menopausal HT.
Despite the widespread opinion from health professionals following the WHI results for women to avoid HT due to high risks without counterbalancing benefit, some doctors remained skeptical of the complete turnaround in recommending HT for women at menopause. Why had the younger nurses followed yearly shown health benefits without medical side effects? Could there be a difference in risk/benefit of HT when it was given to younger women closer to their natural menopause as opposed to women who were older and often 15-20 years removed from their menopause?
NIH was asked for data on women in the study groups who were relatively young and it took over 5 years for NIH to finally analyze this subgroup of women in the WHI who were between 50-59 years old. In fact this age group did demonstrate cardiovascular protection with the use of HT. This new revelation led to the so-called “window of opportunity” theory which proposed that estrogen did provide cardiovascular protection as long as it was given within 10 years of woman’s natural menopause.
Over the past 13 years since the WHI, the breast cancer issue has diminished as a concern as reanalysis of the original data by NIH suggested there was no statistical increase in breast cancer in the study group 1 compared to the control group. This combined with emerging recognition of cardiovascular protection of HT use for younger women has turned the results of the WHI upside down. Moreover, women who had been treated with estrogen only, showed an actual decrease in breast cancer rates. In recent years the focus on a possible culprit for breast cancer in the WHI study group 1 pointed towards the synthetic progestin in Prempro as a possible cause of increased breast cancer occurrence. The synthetic progestin is known as methoxy progesterone acetate or MPA or Provera. A large study group in France using bioidentical progesterone in women demonstrated no increased in breast cancer in women on HT for over 10 years.
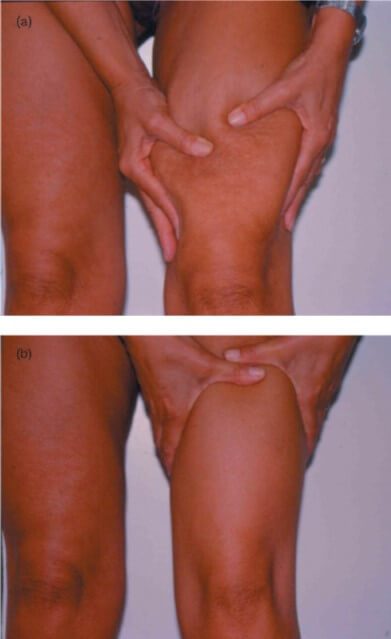
The incidence of blood clots seems also related to the type and method of estrogen administration. Taking estrogen through the skin or transdermally has been shown to be safe compared to oral estrogen which is associated with the risk of blood clots. The WHI used oral estrogen and in the study groups. Of note, only estradiol, a bioidentical estrogen, can be applied to the skin while the non-bioidentical estrogen, Premarin, must be swallowed. Here may also be another advantage of using bioidentical hormones.
Several recent large European epidemiological studies of women on HT around the start of their menopause or within the “window of opportunity”have demonstrated impressive cardiovascular disease protection compared to women who did not use HT at menopause. The studies used bioidentical estradiol however one study also employed the synthetic progestin MPA. Similarly, recent epidemiological studies are now emerging suggesting HT is protective against dementia. Women are affected by Alzheimer’s 3-1 compared to men and the incidence of dementia is increasing every year as women are living longer. Irrational fear of HT at menopause or physician unwillingness to recommend HT may be depriving women of crucial treatments protecting their long term health.
Dr. Terlinsky has been a member of the Endocrine Society and the North American Menopause Society (NAMS) for over 10 years. Attending annual meetings and focusing on the developments in HT for women over the past 13 years has been a major interest of his and it has kept him up to date with respect to developments in the field. Dr. Terlinsky vividly remembers the beginning of the “nuclear winter” for HT following the WHI. He has seen and read the initial post WHI guidelines from such respected medical organizations as the American College of Obstetrics and Gynecology, The Endocrine Society, the American Association of Clinical Endocrinologists, the American College of Physicians, International Menopause Society, the North American Menopause Society (NAMS), and U.S. Preventive Services Task Force. Those initial 2002-2003 guidelines were virtually in lockstep with one another with the exception of the International Menopause Society as they proclaimed HT was dangerous and had little benefit. The International Menopause Society has always been skeptical of the dire findings associated with HT which came from the WHI. It has been recommending the use of HT for long-term health benefits for women since at least 2011.
Dr. Terlinsky is cognizant of the revisions in guidelines for HT for women made by many of the above-mentioned medical organizations over the years since 2002 as new research information has accumulated. With the exception of the International Menopause Society none of the above-mentioned societies has openly reversed their position about advising HT for women at menopause for long-term health benefit.
But there is breaking news on the HT front. Data from Finland was presented at the most recent North American Menopause meeting once again demonstrating long-term benefit for women who take HT at menopause. The North American Menopause Society is likely to change its position on the use of HT for long-term benefit as the “nuclear winter” of hormone therapy slowly lifts. It is expected that the North American Menopause Society will likely join the International Menopause Society in recommending hormone therapy for some women for long-term health benefit and chronic disease prevention particularly if hormone therapy is started within the “ window of opportunity” years mentioned above. Those new recommendations are likely to be issued in early 2016.
Unfortunately, many physicians and allied health care providers have been discouraging women from taking hormones for years, and an entire generation of providers has been trained and indoctrinated into being, “anti-hormone”. This has caused women to be offered advice that is not based on current, up to date information regarding menopause hormone therapy. A good example of the unintended consequences of the 2002 post WHI entrenched recommendations today is the published data which estimates an extra 70,000 postmenopausal osteoporotic bone fractures annually that could have been prevented by hormonal treatment for osteoporosis protection. Many women with fractures had declined hormone therapy at their menopause on account of fear which was not counted by current information from the providers. As mentioned above emerging data also suggests women are allowing themselves to be at a much higher risk of dementia, stroke, and heart attack by not considering hormone therapy at menopause.
The real problem is another long-term large prospective trial as needed to once again assess recommending and providing women with hormone therapy at menopause and observing the beneficial effects over decades. That trial also needs to answer the question of whether bioidentical hormones hold advantages over synthetic hormone. For a variety of reasons this is unlikely to occur so that physicians who want to offer women the very best recommendations regarding hormone therapy must provide menopausal women with the best current data along with a scientific explanation of the preponderance of evidence that is now available. In subsequent articles on his website Dr. Terlinsly will explore other related topics dealing with menopausal hormone therapy.